PEG tube placement
Key facts
- A PEG tube is a feeding tube that’s placed into your stomach.
- It’s used when you are unable to eat enough or swallow safely.
- The PEG tube is way to supplement your diet — you may need the PEG tube for all feeding.
- The PEG tube is placed during the short procedure where a hole is created in your stomach.
What is a PEG tube?
A PEG tube is a feeding tube placed into your stomach. It allows liquid nutrition (food), fluids and medicine to go straight into your stomach.
PEG stands for percutaneous endoscopic gastrostomy:
- percutaneous (through the skin)
- endoscopic (via an endoscope)
- gastrostomy (to the stomach)
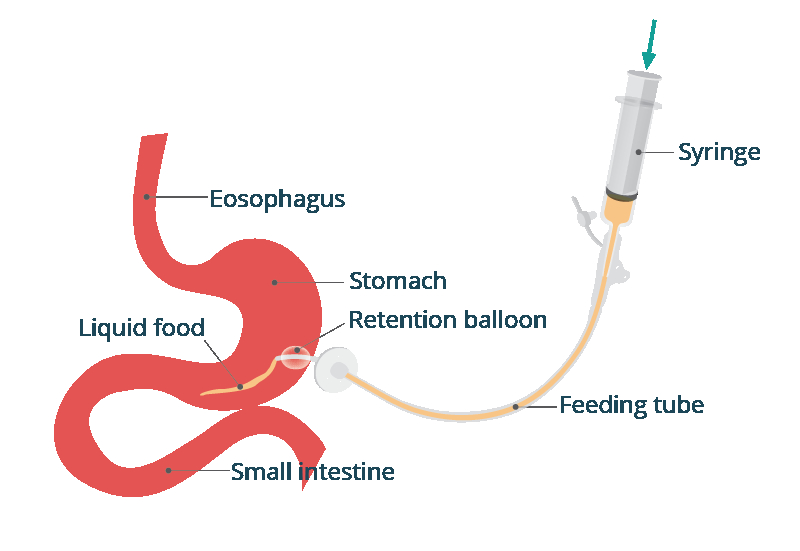
During the procedure a hole is made from your abdominal (tummy) wall into your stomach. Then a feeding tube is placed in the hole.
A PEG tube is made from silicone. The tube can last up to a year before being replaced.
When is a PEG tube needed?
A PEG tube is used by people who are unable to eat or drink enough by mouth. Some people who have difficulty chewing or swallowing may also use a PEG tube.
Reasons for PEG tube placement include:
- problems of the oesophagus or face
- a brain injury, such as a stroke
- surgery of the head and neck area
- a long-term illness, such as cancer
- an eating disorder
- medical conditions, including multiple sclerosis and Parkinson’s disease
How to prepare for a PEG tube placement
After doing a physical examination, your doctor is likely to:
- do blood tests and urine tests
- do an x-ray of your stomach
- review your medicines
- use an endoscope to examine the inside of your stomach
If you take blood thinners including aspirin, these will be stopped for a few days.
You will need to fast (not eat food or drink liquid) for 6 hours before the procedure. You should arrange for someone to take you home afterwards.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
What happens during a PEG tube placement
If you are having a PEG tube placement:
- You will usually be given medicine (a sedative) to help you relax.
- You will probably also have a local anaesthetic so you can swallow the endoscope more easily. Children may need a general anaesthetic.
- A mouth guard is used to protect your teeth and the endoscope.
- The endoscope is inserted through your mouth into your stomach. It’s used to find the best place in the stomach for the PEG tube.
- Then the skin under the ribs is numbed with local anaesthetic so a small cut can be made where the PEG tube will exit your body.
- A wire is passed through the cut and into your stomach at the position marked by the endoscope. The endoscope grips the wire and pulls the wire up to your mouth. The PEG tube is then attached to the wire.
- The wire is then used to draw the PEG tube from your mouth to your stomach, through the stomach wall and through the abdomen at the cut under your ribs.
By the end of the procedure, one end of the PEG tube will sit in your stomach and the other will sit against your skin.
The whole procedure usually takes 20 to 30 minutes. You will be given antibiotics to lessen the risk of infection.
Recovering from PEG tube placement
You might or might not be allowed to go home the same day.
It is common to have some pain in the throat for a few days. The area on your abdomen where the tube is placed may be sore for a week.
You will receive pain relief if needed. You might also have:
Your doctor will check the tube is in the correct position before you can use it.
After 6 to 24 hours, you will be given clear fluids through the PEG tube. Once you are used to this, other feeds and medicines can be given this way.
Before leaving hospital, you will receive training on how to use the PEG tube. The feed can be given continuously (by pump) or at intervals (by a syringe driver or flask). Your dietitian will recommend a suitable liquid feed to meet your needs.
Depending on your condition, you can continue to eat and drink by mouth. The PEG tube is way to supplement your diet. However, some people need the PEG tube for all feeding.
You can remain on PEG feeding long term. If you no longer need PEG feeding the tube can be removed. A simple procedure is performed to repair the hole in your abdomen.
What are the risks of PEG tube placement?
Problems are rare, however the risks include:
- infection or bleeding in your abdomen
- chest infection — caused by aspiration (fluid going into your lungs)
- a tear in your oesophagus (food pipe), stomach or small bowel
- a blockage in the tube, by food residue or medications
- the tube might move or accidentally fall out
If your tube moves, another tube should be placed as soon as possible. This is to stop the hole from closing.
Medicines can be given through the PEG tube however care is needed as some medicines can block the tube. Blockages can be prevented by flushing the tube after each use. Some medicines need to be prepared specially to be given through a PEG tube.
Your pharmacist may change some of your medicines to a liquid so they can be given safely.
Contact your doctor without delay if you have:
- signs of infection (fever and/or chills)
- redness, severe pain, swelling, a lot of bleeding or fluid leaking around the PEG tube
- headaches or muscle aches
- feeling dizzy or unwell
- nausea or vomiting
- constipation
- swollen belly
Resources and support
Visit the healthdirect surgical procedures page to learn more about surgical procedures, with information covering:
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: February 2024